Cancer Genomics
Genomics refers to the study of how genetic information about a cancer influences how that tumor is treated. The modern classification of breast cancers was developed in 2000 with the discovery of four genetic tumor types. Each type of breast cancer is really a separate disease and is treated differently. The following discussion applies to invasive cancers only (stage 1-4). Non-invasive ductal carcinoma-in-situ (DCIS) is not treated based on genomic typing.
Why treat based on tumor type?
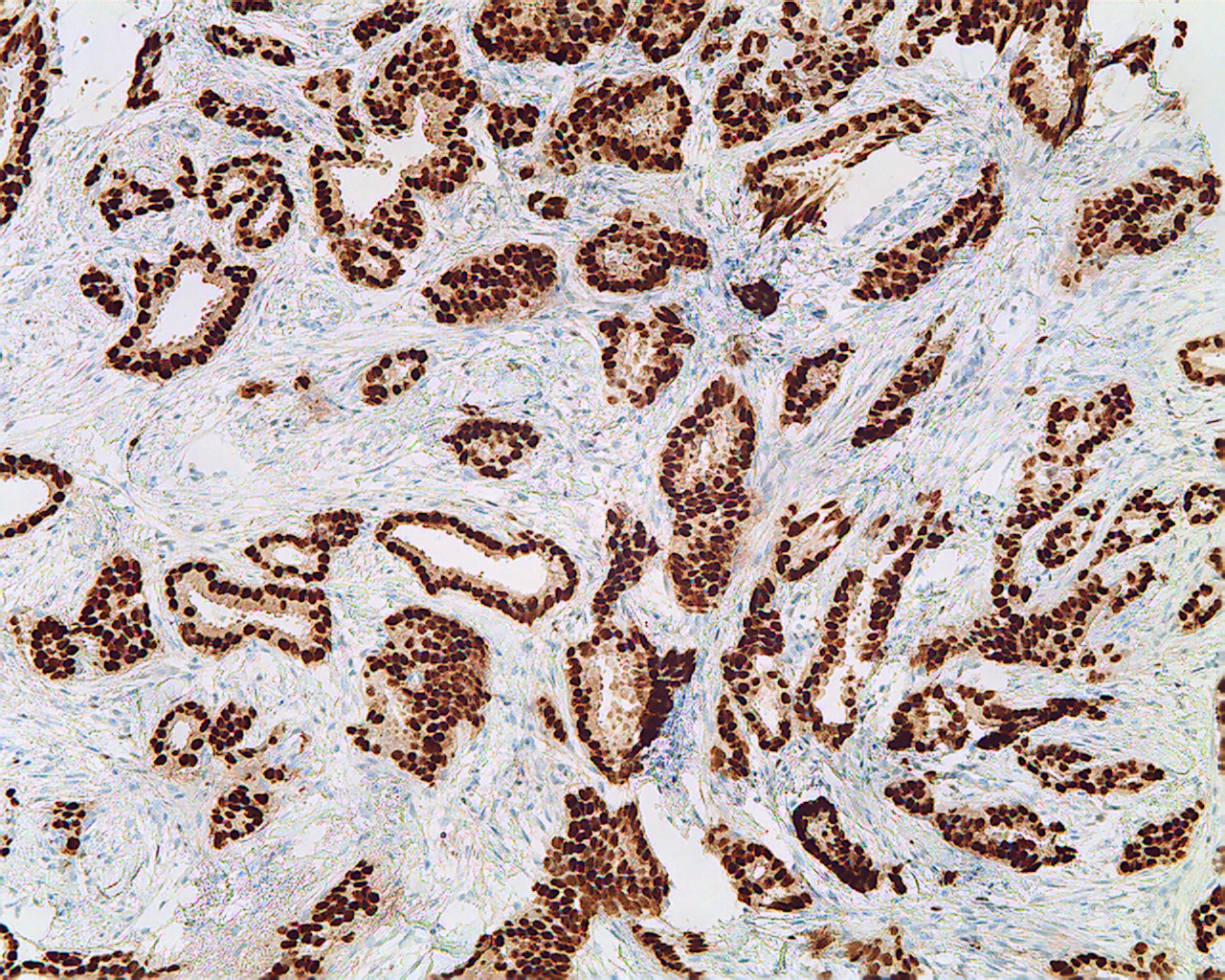
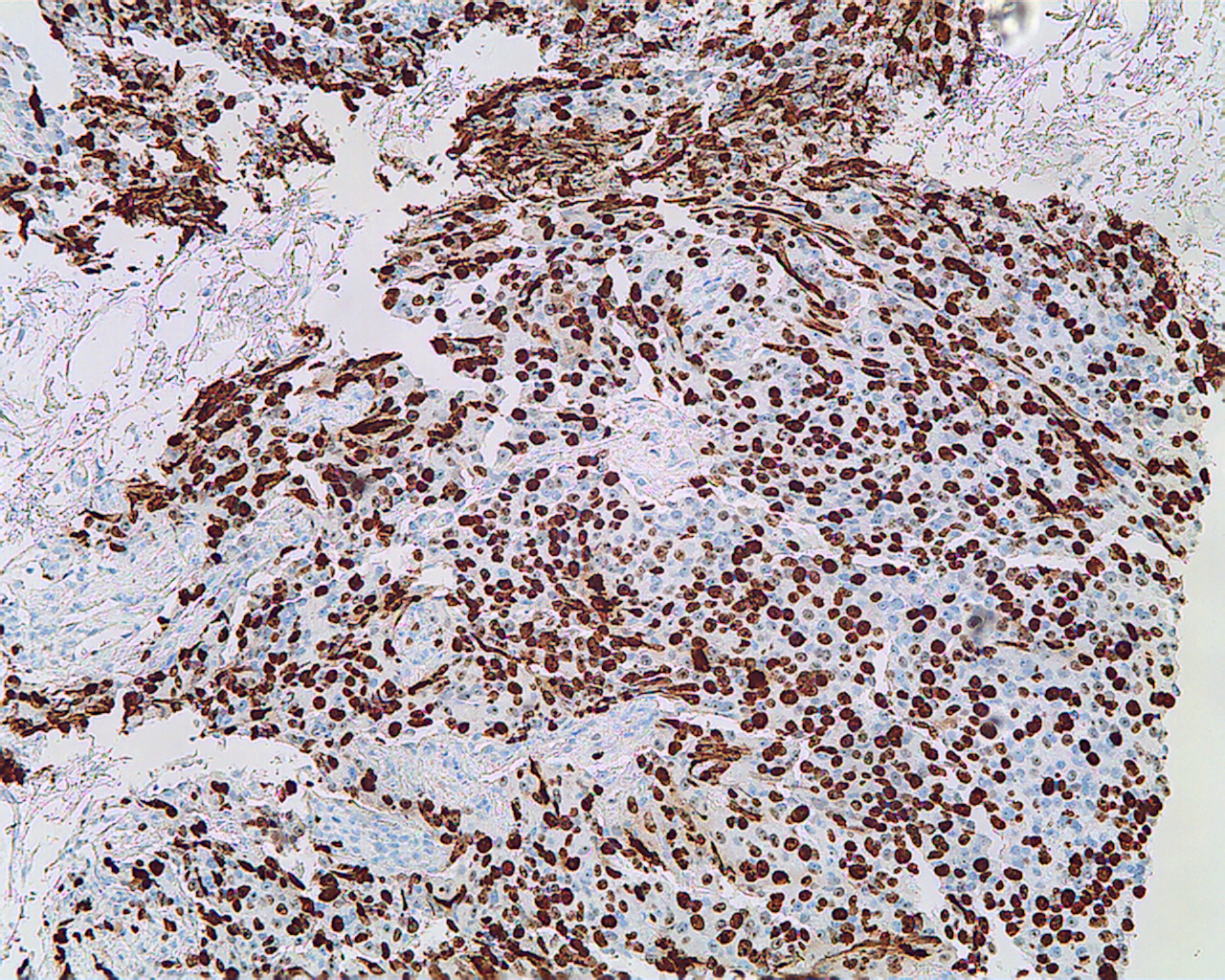
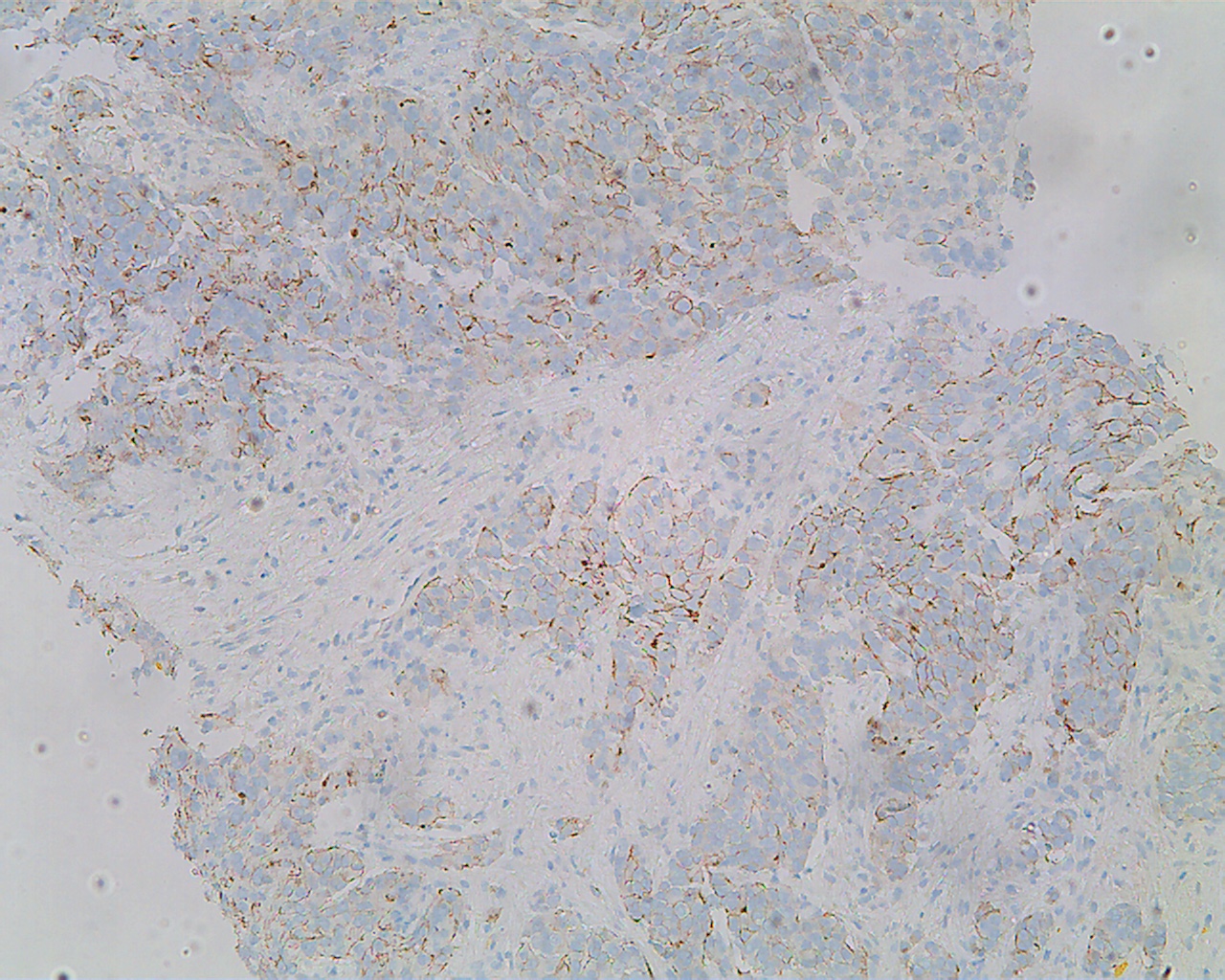
The reason we treat breast cancers based on their tumor type is simple. It works. Traditionally, characteristics of the tumor were determined through a microscopic staining process called IHC (immunohistochemistry). IHC was a big advance in its day. Tumors that respond to estrogen, have abnormal cell surface receptors, or were more aggressive, could be identified with IHC. This lead to better treatments that have improved survival.
Genomic tumor typing has taken this one step further. The characteristics of the tumor that are seen on IHC are better seen through an analysis of the tumor's DNA. The bottom line is that genomic tumor analysis better predicts the response of the tumor to different treatments better than IHC does. And response is what it's all about. When a tumor responds to treatment, people with cancer live longer and suffer less.
The different cancer types shown by genomic analysis are listed below.
Luminal A
Luminal A cancers are the most common tumor type. About 62% of cancers are Luminal A. Luminal A cancers are slow growing and not very aggressive. For this reason, they are sometimes referred to as low-risk tumors. Some of them are ultralow-risk cancers that require only minimal treatment. Luminal A cancers also do not respond to traditional chemotherapy. For this reason, Luminal A cancers are not treated with chemotherapy. That's right. Over 60% of breast cancers don't need chemotherapy; a result that has come out of genomic cancer research. Recurrence rates, without chemotherapy, are less than 10% at 10 years.
Treatment Sequence:
Surgery
Radiation (not always)
Antiestrogen therapy (not in ultralow-risk)
Luminal B
Luminal B cancers are similar to luminal A cancers, but are more aggressive. About 20% of tumors are luminal B. Luminal B tumors respond to standard chemotherapy, an important part of their treatment. Recurrence rates, without chemotherapy, are up to 30% at 10 years.
Treatment Sequence:
Surgery
Chemotherapy
Radiation (not always)
Antiestrogen therapy
HER2-Enriched
HER2-enriched tumors have more than the usual amount of the HER2 protein receptor on the surface of their cells. This causes these cancers to grow and metastasize aggressively. HER2-enriched tumors comprise about 7% of cancers, and respond very well to biologic therapy directed against the abnormal cell surface HER2 receptors. Some biologic treatments for HER2-enriched cancers are available only when chemotherapy is used before surgery. This is called neoadjuvant chemotherapy. As a result, chemotherapy is given first in many of these cancers. Recurrence rates, without chemotherapy, are up to 30% at 10 years.
Treatment Sequence:
Chemotherapy with anti-HER2 biologic therapy
Surgery
More anti-HER2 biologic therapy
Radiation (not always)
Antiestrogen therapy (not always)
Basal-Like
Basal-like cancers comprise about 10% of cancers. They are more common among large cancers (another reason why screening is important). Basal-like cancers are more difficult to treat, because most of them do not have an easily accessible biologic target like other cancers do. As a result, their rate of recurrence is higher. Some are associated with BRCA1 genetic susceptibility mutations. They are also a mixed group of tumors, exhibiting a wide variety of responses to treatment. About 40% do not respond to standard chemotherapy. As a result, they are usually treated with chemotherapy prior to surgery so that their response to chemotherapy can be observed on the tumor itself. Recurrence rates, without chemotherapy, can exceed 30% at 10 years.
Treatment Sequence:
Chemotherapy
Different Chemotherapy (if tumor response is poor)
Surgery
Radiation (not always)